Job Description
Under the direction of the Director of Quality/Performance Improvement, the role is responsible for thedevelopment, implementation and facilitation of processes related to the peer review of cases, tracking andtrending of data and maintenance of appropriate files to determine whether appropriate care was delivered inaccordance with the Medical Staff Constitution, Medical Staff General Rules and Regulations, Hearing Manual,accreditation, regulatory and licensing requirements. The QI Coordinator (Case Review - CRC) applies clinicalexpertise and independent judgment in analyzing patient cases, identifying and pursuing presenting issues andfacilitating case presentation meetings monthly to the Chief Medical Officer and Vice President of Medical Affairs.
This role leans on clinical background to review plans of care delivery, identifying and escalating potential concerns and providing consultative services and guidance to medical/legal affairs and departmental/divisional leadership as needed. CRC's exercise significant discretion in independently analyzing high-volume, time sensitive case reviews – producing legal correspondence and maintaining all required documentation/record keeping required as the case review is completed.
Primary Duties & ResponsibilitiesEstablishes, in collaboration with Department Chairs and Clinical Chiefs, and assures that comprehensive screening and peer review criteria are maintained and consistently employed for assigned medical staff areas. Utilizes appropriate resources, literature and clinical expertise when establishing and reviewing criteria. Ensures that criteria meets regulatory, accreditation and licensing requirements.
Assures that the appropriate cases are identified and retrieved for peer review. Sets up appropriate systems to capture (i.e., using logs, special data retrieval, MIDAS, etc.) and retrieve cases.
Monitors data and peer review outcomes for any trends by MD, indicator or department and facilitates appropriate notification, review and action when trends are identified.
Coordinates and facilitates the review of cases by physicians and/or appropriate committees to determine whether appropriate care was delivered within established timeframes per department/medical staff policy. Presents findings to medical leadership, communicating essence of the case from a clinical practices perspective
Assures that peer review work sheets and electronic MIDAS worksheets are completed with appropriate codes, documentation, justification, signatures and back-up documents.
Prepares all written documentation necessary to obtain information (i.e. inquiry letters), communicate case review outcomes (i.e. educational letters), or document case review actions (follow-up letters) as needed. Assures timely response for all correspondence and documentation requests in cooperation with Department Chair and Clinical Chief.
Creates and maintains physician profiles and files that are complete and meet department standards. Assures that all case reviews and documents are filed in the Physician’s Quality File and that the MIDAS database captures all cases reviewed.
Performs accurate and timely data entry of peer review outcomes into the appropriate databases (i.e. MIDAS).
Facilitates, creates and/or produces statistical and other reports summarizing any case review or peer review activities in accordance with standard department formats. Facilitates the production, review and presentation of Case Review Summaries to the appropriate Committees.
Establishes and maintains uniform, organized filing system and database records. At the direction of management researches, gathers, sorts, compiles and organizes information from the files, from other departments and offices, from outside agencies, etc., for special reports and information requests.
Qualifications
Education:
- Bachelor’s degree in nursing required
Experience and Skills:
- 2 years of prior nursing experience in an acute care setting required
- 1 year minimum experience in a quality improvement/peer review role, strongly preferred.
- Experience in word processing required
- Experience in demonstrating the ability to handle multiple tasks frequently with short timelines, to prioritize and organize work, and to complete assignments in a timely manner preferred.
Licenses and Certifications:
- Active California Registered Nurse License – upon time of hire required
Physical Demands:
- Perform continuous operation of a personal computer for four hours or more.
- Use hands and fingers to handle and manipulate objects and/or operate equipment.
Req ID : 6710
Working Title : Quality Improvement Specialist -Peer Rev Quality Svc Pt Safety
Department : Peer Rev Quality Svc Pt Safety
Business Entity : Cedars-Sinai Medical Center
Job Category : Compliance / Quality
Job Specialty : Qual Measurement & Reporting
Overtime Status : EXEMPT
Primary Shift : Day
Shift Duration : 8 hour
Base Pay : $120,224 - $192,358
Our compensation philosophy
We offer competitive total compensation that includes pay, benefits, and other recognition programs for our employees. The base pay range shown above takes into account the wide range of factors that are considered in making compensation decisions including knowledge/skills; relevant experience and training; education/certifications/licensure; and other business and organizational factors. This base pay range does not include our comprehensive benefits package and any incentive payments that may be applicable to this role. Pay Transparency Non Discrimination Provision (PDF) (opens in new window)
Diversity and Inclusion at Cedars-Sinai
We are caretakers and innovators committed to the pursuit of equitable healthcare. But health equity is not possible without representation. Our commitment to diversity goes beyond demographics or checking boxes. Our people must reflect the diverse identities, experiences and geographies of the communities and patients we serve – because that’s what our patients, colleagues and communities deserve. Quality Care and Research—For All, By All (opens in new window).
Cedars-Sinai is an Equal Employment Opportunity employer.
Cedars-Sinai does not unlawfully discriminate on the basis of the race, religion, color, national origin, citizenship, ancestry, physical or mental disability, legally protected medical condition (cancer-related or genetic characteristics or any genetic information), marital status, sex, gender, sexual orientation, gender identity, gender expression, pregnancy, age (40 or older), military and/or veteran status or any other basis protected by federal or state law. If you need a reasonable accommodation for any part of the employment process, please contact us by email at Applicant_Accommodation@cshs.org and let us know the nature of your request and your contact information. Requests for accommodation will be considered on a case-by-case basis. Please note that only inquiries concerning a request for reasonable accommodation will be responded to from this email address.
Cedars-Sinai will consider for employment qualified applicants with criminal histories, in accordance with the Los Angeles Fair Chance Initiative for Hiring.
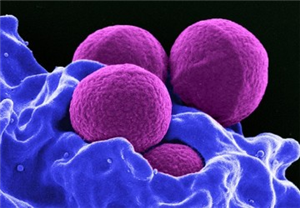
At Cedars-Sinai, we are dedicated to the safety, health and wellbeing of our patients and employees. This includes protecting our patients from communicable diseases, such as influenza (flu) and COVID-19. For this reason, we require that all new employees receive a flu vaccine based on the seasonal availability of flu vaccine (typically during September through April each year) as a condition of employment, and annually thereafter as a condition of continued employment, subject to medical exemption or religious accommodation. For the same reason, you may also be required to receive other vaccines such as COVID-19 as a condition of employment. Cedars-Sinai reserves the right to make modifications to its required list of vaccines as required by law and/or policy. Cedars-Sinai’s AA Policy Statement (PDF) (opens in new window)