Job Description
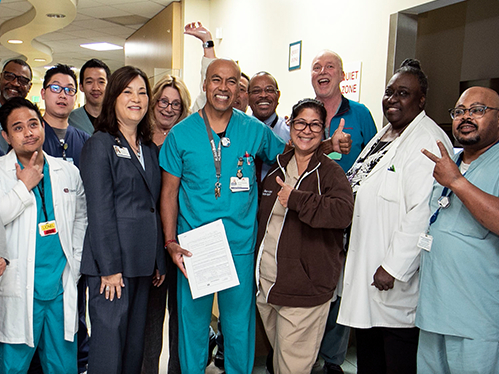
Align yourself with an organization with a reputation for excellence! Cedars-Sinai was awarded the National Research Corporation’s Consumer Choice Award 19 times for providing the highest-quality medical care in Los Angeles. We were also awarded the Advisory Board Company’s Workplace of the Year. We offer an outstanding benefits package that includes healthcare and a generous time-off policy, in addition to competitive compensation. Join us! Discover why U.S. News & World Report has named us one of America’s Best Hospitals.
What will I be doing in this role?
Under general supervision and following established practices, policies, and guidelines, provides patient relations support to Patient Financial Services, performing duties which include identifying, analyzing, resolving and responding to customer inquiries, concerns and issues, and following up on accounts to ensure payment and resolution. Positions at this level require advanced knowledge in specialized functions and a full understanding of the revenue cycle. You will work independently and have strong customer service skills and work well with patients, deescalate issues quickly, able to talk, think and access the system to achieve maximum customer satisfaction. This position requires strong analytic and prioritization skills and the ability to understand, interpret and explain payor contracts and CSMC billing and collections policy and practices. This position may be cross-trained in other revenue cycle functions and provide back-up coverage.
- Applies detailed knowledge of and follows all hospital and department policies, procedures (e.g., PHI, PFS employee handbook).
- Demonstrates detailed knowledge of Cedars-Sinai’s core patient accounting systems and/or department specific systems and uses them effectively and efficiently.
- Effectively monitors assigned work queues and workload, ensuring resolve of accounts in a timely and accurate manner. Takes initiative on issues and/or problems by advancing them to the supervisor.
- Adheres to documentation standards of the department. Accurately uses activity codes. Notes are clear and concise. Correctly enters data in fields. Maintains acceptable levels of speed and accuracy.
- Completes all necessary research and account follow-up activities to resolve inquiries and/or customer complaints. Ensures that the resolution completed meets the patient’s needs.
- Responds to patient, insurance company and other authorized third-party inquiries, including return of calls and research needed to bring account to final resolution.
- Negotiates and documents payment plans within established policies.
- Achieves timely and accurate account collection for hospital and professional services. Responsible for initiating collection calls to patients and insurance companies to collect on unresolved accounts. Maintains A/R per department protocol. Reviews accounts on continuing basis and refers uncollectible accounts to collection agency or attorney on a timely basis. Ensures account is routed to appropriate work queue for approval.
- Responds timely, effectively, and appropriately to deliverables.
- Shares knowledge, time, and expertise to assist other members of the team.
- Ensures practices and procedures are inclusive of interpersonal and cultural diversity.
- Identifies and responds appropriately to both internal and external customer needs using available resources.
Qualifications
Requirements:
- High School Diploma/GED required. Associate degree in business administration or another related major or college level courses in finance, business, or health insurance preferred.
- A minimum of 1 year of hospital billing or professional billing and/or Collection experience with customer service and call center experience required.
Why Work Here?
Beyond outstanding employee benefits including health and dental insurance, vacation, and a 403(b) we take pride in hiring the best employees. Our accomplished staff reflects the culturally and ethnically diverse community we serve. They are proof of our commitment to creating a dynamic, inclusive environment that fuels innovation.
Req ID : 6566
Working Title : Financial Care Specialist I (Remote)
Department : CSRC Customer Service and Self-Pay
Business Entity : Cedars-Sinai Medical Center
Job Category : Patient Financial Services
Job Specialty : Patient Billing
Overtime Status : NONEXEMPT
Primary Shift : Day
Shift Duration : 8 hour
Base Pay : $25.06 - $37.59
Our compensation philosophy
We offer competitive total compensation that includes pay, benefits, and other recognition programs for our employees. The base pay range shown above takes into account the wide range of factors that are considered in making compensation decisions including knowledge/skills; relevant experience and training; education/certifications/licensure; and other business and organizational factors. This base pay range does not include our comprehensive benefits package and any incentive payments that may be applicable to this role. Pay Transparency Non Discrimination Provision (PDF) (opens in new window)
Diversity and Inclusion at Cedars-Sinai
We are caretakers and innovators committed to the pursuit of equitable healthcare. But health equity is not possible without representation. Our commitment to diversity goes beyond demographics or checking boxes. Our people must reflect the diverse identities, experiences and geographies of the communities and patients we serve – because that’s what our patients, colleagues and communities deserve. Quality Care and Research—For All, By All (opens in new window).
Cedars-Sinai is an Equal Employment Opportunity employer.
Cedars-Sinai does not unlawfully discriminate on the basis of the race, religion, color, national origin, citizenship, ancestry, physical or mental disability, legally protected medical condition (cancer-related or genetic characteristics or any genetic information), marital status, sex, gender, sexual orientation, gender identity, gender expression, pregnancy, age (40 or older), military and/or veteran status or any other basis protected by federal or state law. If you need a reasonable accommodation for any part of the employment process, please contact us by email at Applicant_Accommodation@cshs.org and let us know the nature of your request and your contact information. Requests for accommodation will be considered on a case-by-case basis. Please note that only inquiries concerning a request for reasonable accommodation will be responded to from this email address.
Cedars-Sinai will consider for employment qualified applicants with criminal histories, in accordance with the Los Angeles Fair Chance Initiative for Hiring.
At Cedars-Sinai, we are dedicated to the safety, health and wellbeing of our patients and employees. This includes protecting our patients from communicable diseases, such as influenza (flu) and COVID-19. For this reason, we require that all new employees receive a flu vaccine based on the seasonal availability of flu vaccine (typically during September through April each year) as a condition of employment, and annually thereafter as a condition of continued employment, subject to medical exemption or religious accommodation. For the same reason, you may also be required to receive other vaccines such as COVID-19 as a condition of employment. Cedars-Sinai reserves the right to make modifications to its required list of vaccines as required by law and/or policy. Cedars-Sinai’s AA Policy Statement (PDF) (opens in new window)